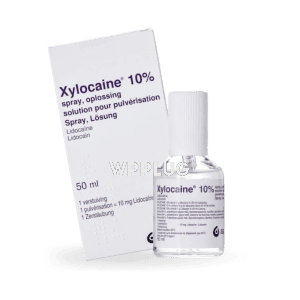
Xylocaine
| Product dosage: 50 gm | |||
|---|---|---|---|
| Package (num) | Per tube | Price | Buy |
| 8 | 7.31 $
Best per tube | 84.24 $ 58.50 $ (31%) | 🛒 Add to cart |
| 10 | 10.53 $ | 105.30 $ (0%) | 🛒 Add to cart |
Synonyms | |||
Xylocaine: Expert Local Anesthesia for Procedural Pain Control
Xylocaine (lidocaine hydrochloride) is a premier amide-type local anesthetic agent, established as a cornerstone in medical practice for its rapid onset and reliable duration of action. It is formulated to provide effective nerve blockade, facilitating a wide range of diagnostic and therapeutic procedures with enhanced patient comfort. Its well-understood pharmacokinetic and pharmacodynamic profile makes it a trusted choice for clinicians worldwide, ensuring predictable and manageable anesthesia for both infiltration and regional nerve block techniques.
Features
- Active Pharmaceutical Ingredient: Lidocaine Hydrochloride.
- Available in multiple concentrations (e.g., 0.5%, 1%, 2%) and formulations, including solutions for injection, topical gels, ointments, and sprays.
- Rapid onset of anesthetic action, typically within 2-5 minutes for infiltration.
- Intermediate duration of efficacy, generally lasting 30-90 minutes depending on the concentration, vascularity of the site, and addition of a vasoconstrictor like epinephrine.
- Sterile, pyrogen-free solutions for injection, ensuring patient safety.
- Precisely buffered to a pH compatible with tissue tolerance, minimizing injection discomfort.
Benefits
- Provides rapid and profound local anesthesia, enabling pain-free execution of minor surgical, dental, and dermatological procedures.
- Enhances patient cooperation and satisfaction by significantly reducing procedural anxiety and discomfort.
- Allows for precise anatomical localization of pain via nerve blocks, aiding in both diagnosis and treatment.
- Improves procedural efficiency for healthcare providers by creating optimal working conditions.
- Offers a favorable safety margin when administered correctly and within recommended dosage guidelines.
- Versatile application across numerous medical specialties, from emergency medicine to outpatient clinics.
Common use
Xylocaine is indicated for the production of local anesthesia by infiltration injection, peripheral nerve block, and central neural techniques including epidural and spinal blocks (specific to approved formulations). Its common applications include, but are not limited to: suturing of lacerations; incision and drainage of abscesses; dental procedures such as restorations and extractions; dermatological surgeries; diagnostic procedures like lumbar puncture; and as a topical anesthetic for mucous membranes to facilitate endoscopic examinations or intubation.
Dosage and direction
Dosage varies significantly based on the procedure, tissue vascularity, area to be anesthetized, and patient’s physical status. The smallest dose and lowest concentration that provides effective anesthesia should always be used.
- For Infiltration and Minor Nerve Blocks: Maximum recommended dose is 4.5 mg/kg (not to exceed 300 mg) of plain lidocaine. With epinephrine (1:100,000 to 1:200,000), the maximum dose is 7 mg/kg (not to exceed 500 mg).
- Administration: Aspirate before and during injection to avoid intravascular administration. Inject slowly. Doses must be tailored for debilitated, elderly, or acutely ill patients and for children, based on body weight.
- Always refer to the specific product monograph for detailed, procedure-specific dosing instructions. The following is a general guide:
- Simple Infiltration & Dental: 1-5 mL of a 1% or 2% solution.
- Minor Nerve Blocks (e.g., Digital): 1-5 mL of a 1% or 2% solution (use extreme caution, avoid epinephrine-containing solutions for digital blocks).
- Epidural: A test dose of 2-3 mL of a 1.5% or 2% solution is standard to rule out subarachnoid or intravascular placement.
Precautions
- Use with extreme caution in patients with known drug sensitivities, severe shock, or heart block.
- Administer with care and at reduced doses in areas of poor vascularization (e.g., digits, nose, ears, penis) due to the risk of ischemic injury or sloughing, particularly when using vasoconstrictors.
- Caution is advised in patients with hepatic impairment, as lidocaine is metabolized by the liver.
- Cardiovascular and respiratory vital signs must be monitored continuously during major nerve blocks.
- Resuscitative equipment and drugs for managing adverse reactions (e.g., convulsions, cardiac arrest) must be immediately available.
- Not for ophthalmic use unless specifically formulated and labeled for such.
Contraindications
- Hypersensitivity or allergy to lidocaine hydrochloride, other amide-type local anesthetics, or any component of the formulation.
- Administration of solutions containing vasoconstrictors (e.g., epinephrine) is contraindicated in areas supplied by end-arteries (e.g., digits, penis) and for intravenous regional anesthesia (Bier’s Block).
- The presence of sepsis or severe infection at the proposed injection site.
- Severe degrees of heart block, Adams-Stokes syndrome, or Wolff-Parkinson-White syndrome (for IV antiarrhythmic use; caution with regional anesthesia).
Possible side effect
Adverse reactions are generally dose-related and result from high plasma levels due to excessive dosage, rapid absorption, inadvertent intravascular injection, or hypersensitivity.
- Central Nervous System: Nervousness, dizziness, blurred vision, tremors, drowsiness, convulsions, unconsciousness, and respiratory arrest.
- Cardiovascular: Hypotension, bradycardia, arrhythmias, and cardiovascular collapse, which can lead to cardiac arrest.
- Allergic Reactions: Urticaria, angioedema, bronchospasm, and anaphylactoid reactions, though true IgE-mediated allergy is rare.
- Other: Nausea, vomiting, tinnitus, metallic taste, numbness of the tongue and perioral region, and persistent paresthesia (rare).
Drug interaction
- Antiarrhythmics: Concurrent use with other Class IB antiarrhythmics (e.g., mexiletine) may have additive cardiotoxic and neurotoxic effects.
- Beta-blockers (e.g., propranolol) and Cimetidine: May reduce hepatic blood flow and inhibit lidocaine metabolism, potentially leading to increased plasma levels and toxicity.
- Vasopressors: Can potentiate the pressor effect of sympathomimetic drugs like epinephrine, which may be added to Xylocaine.
- CYP3A4 Inhibitors (e.g., certain antifungals, macrolide antibiotics): May decrease the metabolism of lidocaine, increasing the risk of adverse effects.
Missed dose
The concept of a “missed dose” is not applicable to Xylocaine, as it is administered as a single procedure-based treatment and not on a scheduled dosing regimen. Anesthesia is administered once, as needed for a specific intervention.
Overdose
Overdose manifests primarily as effects on the central nervous and cardiovascular systems.
- Symptoms: Initially may include CNS excitation (restlessness, tremors, convulsions) followed by CNS depression (drowsiness, coma, respiratory arrest). Cardiovascular symptoms include hypotension, bradycardia, arrhythmias, and cardiac arrest.
- Management: Management is supportive and focuses on maintaining an airway and supporting ventilation with oxygen and assisted ventilation (intubation if necessary). Benzodiazepines (e.g., diazepam) are first-line for controlling convulsions. Cardiovascular support includes IV fluids and vasopressors for hypotension. Bradycardia may require atropine. Cardiopulmonary resuscitation must be instituted immediately if cardiac arrest occurs.
Storage
- Store at controlled room temperature, 20°-25°C (68°-77°F). Protect from light.
- Do not freeze. Solutions containing epinephrine should be protected from exposure to light.
- Keep all medications out of the reach of children and pets.
- Single-use vials and ampules are for one patient, one procedure only. Discard any unused portion.
Disclaimer
This information is for educational and professional medical purposes only and does not constitute medical advice. It is not exhaustive. The prescriber must consult the full official prescribing information (monograph) for complete details on indications, dosage, warnings, precautions, and interactions before administering Xylocaine. The healthcare professional is solely responsible for selecting an appropriate agent and dose for each patient based on their clinical judgment and a thorough assessment of the individual patient.
Reviews
“Xylocaine remains the gold standard against which all other local anesthetics are measured in our emergency department. Its predictable onset and reliable duration make it indispensable for everything from simple laceration repair to more complex nerve blocks. The wide range of available concentrations allows for precise tailoring to each clinical scenario.” – Head of Emergency Medicine, University Teaching Hospital.
“In dental practice, the rapid onset of action of 2% Xylocaine with epinephrine is critical for patient comfort and efficient workflow. It provides excellent hemostasis and profound pulpal anesthesia, allowing for pain-free procedures. Its safety profile is excellent when used within recommended guidelines.” – DDS, Oral Surgery Specialist.
“As an anesthesiologist, I value the consistent performance of Xylocaine for epidural anesthesia and peripheral nerve blocks. Its well-characterized pharmacokinetics allow for accurate prediction of block duration and systemic absorption, which is paramount for patient safety, especially in obstetric and ambulatory surgery settings.” – MD, Chief of Anesthesiology.